
Proton radiotherapy is a gentle cancer treatment method with minimal side effects. It allows for accurate targeting of the proton beam to the target area (at the location of the original tumor) in the lung, thus minimising exposure of surrounding tissues and organs to radiation. In order to achieve the maximum cancer treatment effectiveness for lung cancer, it is vital to irradiate the tumor with high doses of radiation. Nonetheless, this goal is not often achieved in standard irradiation due to possible damage to the surrounding tissues (healthy tissue toxicity).
That is why our physicians and physicists started using a unique procedure – deep inspiration breath hold (DIBH) technique. This method allows breathing movements to be minimised and thus the tumor to be irradiated with a high dose with maximum accuracy. At the same time, proton therapy minimises exposure of healthy parts of the lung, the second lung, the heart, cardiac vessels and other organs in the mediastinum to radiation. In this way, proton therapy significantly increases the ratio between the chance to control the tumor, i.e. enhanced treatment effect, and the reduction of possible serious adverse effects.
At the Proton Therapy Center in Prague, proton therapy is used to treat:
- non-small cell lung carcinoma (NSCLC);
- patients who have developed a secondary tumour after previous irradiation, such as for breast cancer, in previous years.
DIBH: The Controlled Breathing Method
As respiratory movements may impair the correct and precise execution of proton irradiation, in the treatment of lung cancer we also use the method of controlled breathing. For this, we use the Dyn’R.
The controlled breathing method has been chosen because it is important that the irradiated area of the body and the target volume of the tumor are irradiated the same way during each fraction. Since this irradiated volume varies depending on breathing, we need to ensure that the patient’s body is always in the same position. This is best done by holding their breath at a certain level. To determine this level, the patient first undergoes a controlled breathing training (Dyn’R training).
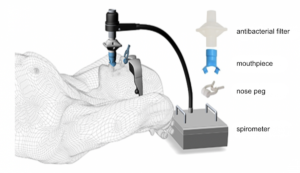
The controlled breathing training is done lying down on the back after being connected to the spirometer, using an antibacterial filter and a mouthpiece. The patient’s nose is held closed by a pin so that all exhaled air flows through their mouth. The patient also wears special glasses, where they see the breathing pattern to follow. The training is conducted by an experienced assistant and the patient has nothing to worry about.
During each irradiation, the patient lies on the radiation table the same way they did during the training, and breathes with the DIBH technique. If the patient accidentally does not manage to hold their breath for the required 20 seconds, they do not have to worry. If they breathe out, the device will detect it and stop irradiation automatically.
Advantages of proton therapy over conventional radiotherapy
One substantial reason to choose proton radiotherapy for lung cancer would be radiation induced heart disease (RIHD). Heart disease caused by radiation is one of the most serious and best-documented very late effects of radiation. Therefore, in the treatment of lung cancer, when radiation is recommended, experts seek to minimise the radiation dose to the heart. Thanks to the proton beam, we are able to significantly reduce the risk of the occurrence of cardiac infarction, cardiac complaints, or the risk of development of pulmonary fibrosis.
Very late effects of lung cancer radiation treatment may be manifested in the tissue of the lungs. According to years of experience, irradiation of larger regions of the lungs is unequivocally linked to the development of pulmonary fibrosis, which consists of changes in the pulmonary tissue. Pulmonary fibrosis can be linked to repeated incidences of pneumonia and chronic cough.
Proton therapy is also suitable for patients who have already undergone a round of radiation for the other breast, for bilateral findings, and is also recommended for patients with associated heart disease.
Proton therapy:
- allows for increasing the overall radiation dose with lower toxicity meaning less strain on critical organs;
- allows for decreasing the radiation dose affecting the healthy tissue of the lungs thereby reducing the risk of emergence of respiratory complaints and the development of pulmonary fibrosis;
- reduces the radiation dose affecting the cardiac muscle thereby reducing the risk of heart disease;
- reduces the risk of the development of swallowing difficulties or loss of appetite;
- allows for enhancing the quality of the patient’s life;
- allows for the use of fewer therapeutic fractions.
|
PROTON IRRADIATION Protons target the tumour directly, sparing healthy tissues and organs from unwanted effects. |
PHOTON IRRADIATION
|
Proton therapy in Prague
In order to choose the optimal treatment, it is important to receive comprehensive and comprehensible information.If radiation is considered as part of your treatment, ask the treating oncologist about all the available irradiation methods as well as treatment-related side effects. These may significantly affect the quality of your life during and after treatment. Our physicians have many years of experience in radiotherapy. Moreover, they are experienced in both standard (photon) and proton radiation therapy and are prepared to answer all of your questions. Do not hesitate to contact us.
The treatment is outpatient, and you come to the Proton Therapy Center for radiation and regular check-ups during treatment. One visit takes about 60 minutes while the radiation is a matter of a few minutes. Prior to each radiation session, we carefully check your position using X-ray scans and carry out certain other checks necessary to commence irradiating. At least once a week, you undergo check-ups with the physician who will go through the treatment progress with you and check your condition.
In most cases, the whole treatment lasts from 25 to 35 business days, according to the regime determined by the physician on the basis of the initial assessment and other diagnostic tests.
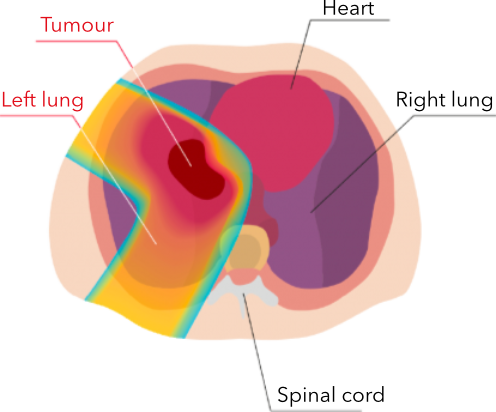
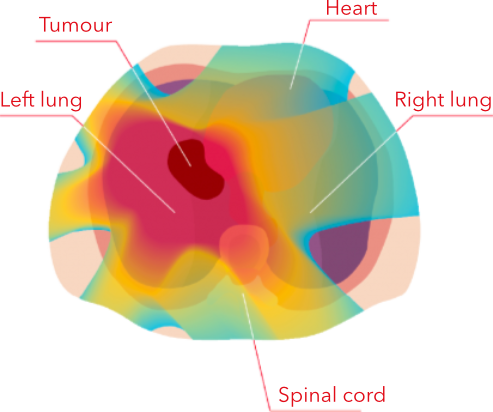 Photons irradiate the tumour as well as the healthy tissues and organs around it.
Photons irradiate the tumour as well as the healthy tissues and organs around it.